Systemic sclerosis: Allogeneic adipose tissue-derived mesenchymal stromal cells grafts
UPhase I/II randomized clinical trial of allogeneic adipose tissue-derived mesenchymal stromal cells systemic infusion in severe systemic sclerosis
ClinicalTrials.gov number : NCT06722105
Funding: PHRC 20-0558
SUMMARY
Acronym: MSC-AT-SSc
Coordinating Investigator:
Professor Dominique FARGE-BANCEL
Internal medicine Unit UF 04, MATHEC Reference Center for autoimmune and rare systemic diseases (FAI2R)
UF 04 Hôpital St-Louis
1, avenue Claude Vellefaux, Paris 75010 Paris
Contact: Pauline LANSIAUX, clinical research engineer, pauline.lansiaux@aphp.fr; Ingrid MUNIA, clinical research coordinator, Ingrid.munia@aphp.fr; +33(0)142385093
Scientific Director:
Professor Karin TARTE
Head of Rennes Immunomonitoring Platform (SITI)
CHU Pontchaillou
2, rue Henri Le Guilloux
Tel: +33 (0)2 232 345 12
Email: karin.tarte@univ-rennes1.fr
Sponsor: Assistance Publique-Hôpitaux de Paris
Justification scientifique:
Systemic sclerosis (SSc) is a rare, severe and chronic systemic autoimmune disease (AD) characterized by vasculopathy, immune dysregulation and fibrosis leading to multi-organ dysfunction (primarily skin, lungs, heart gastrointestinal tract and kidneys), with high morbidity and mortality, altered health-related quality of life, all at high cost for patients and society.
Treatment are mostly symptomatic and only autologous hematopoietic stem cell transplantation (AHSCT) has shown long term improvement in overall and event-free survival with disease-modifying properties. However, AHSCT is contra-indicated in case of advanced visceral involvement and in eligible patients, it is still associated with risk of toxicity. There is an urgent need to identify safe and effective treatments for severe SSc.
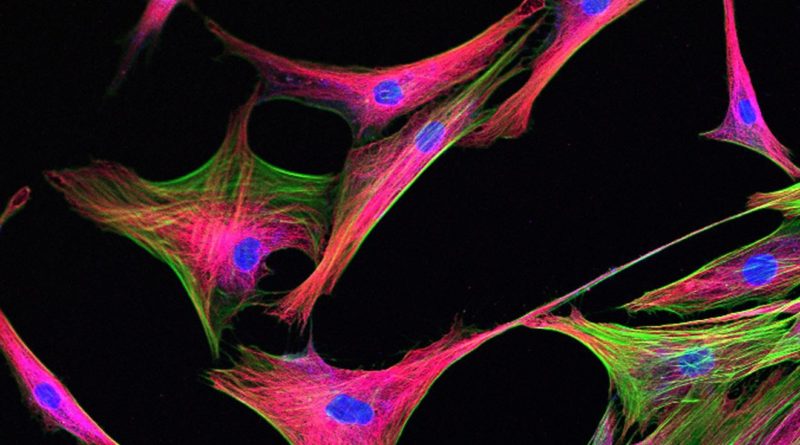
Mesenchymal stromal cells (MSC) are multipotent cells which carry immunomodulatory, pro-angiogenic and anti-fibrotic properties, that can target SSc pathogenesis and its clinical manifestations. The increasing use of MSC, harvested from bone marrow (MSC(M)), adipose tissue (MSC(AT)), or umbilical cord (MSC(UC)) in a variety of indications, provides consistent evidence supporting their safety in humans. The efficacy of MSC(M) intravenous (IV) injection for treating acute graft versus host disease led to their marketing approval in 2012 and MSC(AT) (Alofisel) were approved for severe Crohn’s fistula in 2018.
MSC represent a promising therapeutic approach for SSc. We have previously a) shown disease-specific abnormalities in MSC(M) from SSc patients, providing strong rationale to use allogeneic MSC to treat SSc patients, b) published the first phase I/II dose escalation trial using allogenic MSC(M) infusion in 20 severe SSc patients (ClinicalTrials.gov: NCT02213705, PHRC AOM 11-250) with no safety issues, significant improvement in skin fibrosis at 3 to 6 months after infusion which appeared lower thereafter, thereby supporting the need for repeated infusions.
In vitro, experimental and clinical studies suggest that MSC properties vary according to their tissue of origin/source. We demonstrated that compared to MSC(M), MSC(AT) are easier to harvest and display higher proliferative capability before entering senescence, higher genetic stability, and superior immunosuppressive properties.
Considering the above rationale, we hypothesize that use of healthy donors allogeneic MSC(AT) produced by Etablissement Français du Sang (EFS) will demonstrate a) no safety issues, b) an efficacy profile that will increase with repeated infusion of allogeneic MSC(AT) to treat SSc.
Main objective and primary endpoint
Main objective:
To evaluate the safety one month after allogeneic 2×106 MSC(AT)/kg intravenous administration once or twice at 3 months interval (M0, M3) in severe SSc patients
Primary endpoint: lThe rate of treatment-related Severe Adverse Events (SAE) defined as Adverse Events (AE) of grade equal or above 3 using the NCI Common Terminology Criteria for Adverse Events (CTCAE) v5.0 classification, at one month after each infusion (M1, M4). All adverse events will be adjudicated by a Data and Safety Monitoring Committee.
Secondary objectives and endpoints
Secondary objectives :
1- Safety during the infusion, within the first 24 hours of infusion and during all study follow-up;
2- Efficacy signals to inform future studies, using outcome measures on skin sclerosis, lung function and quality of life, previously validated in SSc or used in other cell therapy trials;
3- Analysis of the response to treatment, Progression-free survival (PFS), Global Rank Composite Score (GRCS) at M3, M6and M12 and ACR Provisional Composite Response Index for Clinical Trials in Early Diffuse Cutaneous Systemic Sclerosis (CRISS) for early SSc patients at M3, M6 and M12;
4- Analysis of the overall survival and assess causes of death;
5- Impact of allogeneic MSC(AT) iv once or twice at 3 months interval on the immune response, including immunophenotyping and alloimmunization up to M6 after starting therapy;
6- Cost effectiveness of the allogeneic MSC(AT) infusion once or twice versus no treatment in severe SSc patients.
Secondary endpoints :
1) Rate of treatment-related SAE defined as AE of grade equal or above 3 CTCAE v5.0 at time and within the first 24 hours of infusion and during all follow-up at: M0, M3, M6, M9 and M12;
2) Main efficacy endpoint: Différence du score cutané de Rodnan modifié (mRSS) entre M0 et M12.
3) Other efficacy disease related endpoints :
a- mRSS at M3, M6 et M9
b- WHO performance status (PS) and Health-Related Quality of Life (HRQoL) questionnaires : Scleroderma-Health Assessment Questionnaire (SHAQ), the Short Form (36) health survey (SF-36v2) and EQ-5D-5L at M0, M3, M6, and M12;
c- Forced Vital Capacity (FVC) and Diffusing capacity of Lung for carbon monoxide (DLCO) at M0, M6 and M12.
4) Response to treatment, defined as any of the following: decreased mRSS > 25%, increased FVC > 10% and/or increased DLCO>10%, without need for further immunosuppression except low dose steroids (below 10mg daily) at M3, M6 and M12;
5) PFS at M12, with progression defined as any of the following: decreased in FVC > 10% or in DLCO > 15%; decrease in LVEF% > 15%; decrease in weight > 15%; decrease in creatinine clearance > 30%; increased mRSS > 25% ; and/or increase in SHAQ> 0.5;
6) GRCS values at M3, M6 and M12;
7) CRISS values for early SSc patients at M3, M6 and M12;
8) Overall survival at M12;
9) Myeloid and lymphocyte sub-populations in all included patients at M0, M1, M3, M4, M6;
10) Alloimmunization in all included patients through the detection and identification of donor-specific anti-HLA antibodies at M0, M3 and M6;
11) Extra-Cost per QALY (quality-adjusted Life Year) gained by unique and repeated IV infusion of allogeneic MSC(AT) in severe SSc after 12 months;
12) Extra-Cost per SAE of grade above or equal to 3 CTCAE avoided by unique and repeated IV infusion of allogeneic MSC(AT) in severe SSc after 12 months;
Design of the trial :Multi-centre, three-arm, randomized, placebo-controlled, double-blind phase I-II trial
Population of trial subjects : Adult patients with refractory severe systemic scleroderma
INCLUSION/EXCLUSION CRITERIA
Inclusion criteria
1- Provide signed and dated informed consent;
2- Willing to comply with all study procedures and be available for the duration of the study;
3- Male or female, aged ≥ 18 and ≤ 70 years of age;
4- SSc patients according to American College of Rheumatology/European League Against Rheumatism (ACR/EULAR) 2013 classification criteria for SSc;
5- Severe disease with either:
a- disease duration of 2 years or less with a modified Rodnan skin score (mRSS) ≥ 20 and (abnormal CRP > 5 mg/l and/or hemoglobin < 11 g/dL), or
b- b) mRSS ≥ 15 without any restriction as to disease duration plus at least one major organ involvement as defined by:
i- respiratory involvement consisting of lung diffusion capacity for carbon monoxide (DLCO) and/or forced vital capacity (FVC) < 80% predicted and evidence of interstitial lung disease (chest X-ray and/or high resolution computed tomography (HRCT) scan) and/or moderate Pulmonary hypertension with baseline resting systolic pulmonary arterial pressures > 35 mmHg and below 50 mmHg by cardiac echocardiography, or mean pulmonary artery pressure > 20 mmHg and < 40 mm Hg on right heart catheterization;
ii- renal involvement consisting of past renal crisis, microangiopathic hemolytic anemia, and/or renal insufficiency not explained by other causes than SSc;
iii- cardiac involvement consisting of reversible congestive heart failure, atrial or ventricular rhythm disturbances such as recurrent episodes of atrial fibrillation or flutter, recurrent atrial paroxysmal tachycardia, 2nd or 3rd degree AV-block, mild to moderate pericardial effusion and/or presence of MRI involvement (Increased T1 or T2 mapping, late gadolinium enhancement, septal D sign) . All causes of organ involvement should be attributed to SSc
6- Contraindication, inadequate response or unwillingness to undergo AHSCT (determined by patient and physician judgement);
7- Contraindication, inadequate response or unwillingness or adverse events necessitating discontinuation of conventional immunosuppressive therapy (MMF, methotrexate);
8- Women of reproductive potential must use highly effective contraception;
9- Men of reproductive potential must use condoms;
10- Health insurance.
Exclusion criteria:
1- Age < 18 years or > 70 years;
2- Pregnancy or unwillingness to use adequate contraception;
3- Life-threatening end-organ damage defined as: DLCO (corrected for hemoglobin) < 30% predicted; Left ventricular ejection fraction < 40% by cardiac echocardiography; Pulmonary hypertension with baseline resting systolic pulmonary arterial pressures > 50 mmHg by cardiac echocardiography, or mean pulmonary artery pressure > 40 mmHg on right heart catheterization; glomerular filtration rate < 30mL/min; 4- Active or chronic Hepatitis (ASAT, ALAT > 3 upper limit normal);
5- Neoplasms of less than 5 years, except for basal cell or in situ cervix carcinoma or concurrent myelodysplasia;
6- Uncontrolled hypertension;
7- Uncontrolled acute or chronic infection;
8- HIV-1 or HIV-2 infection;
9- BMI < 16.5 kg/m2; 10- Severe psychiatric disorder;
11- Bone marrow insufficiency, defined as neutropenia < 1 x 109/L, thrombopenia < 50 x 10^9/L, anemia < 8 g/dL, lymphopenia < 0,5 x 10^9/L 12- Inability to provide informed consent;
13- Patient included in another interventional clinical trial;
14- Patient under tutelle.
Investigational medicinal product(s) :
Allogeneic Adipose tissue derived-MSCs (MSC(AT)) or placebo will be injected by slow intravenous infusion according to the recipient body weight and to the study experimental arms:
– arm 0 : placebo at M0 and M3
– arm 1:1 MSC(AT) (2×10^6 cells/kg) injection at M0 and 1 placebo injection at M3
– arm 2: 1 MSC(AT) (2×10^6 cells/kg) injection at M0 and 1 MSC(AT) (2×10^6 cells/kg) injection at M3
Each allogeneic MSC(AT) is administered intravenously over a 45 min to 1h infusion.
Second infusions of drug product (MSC/placebo) will be performed only in the absence of treatment-related Severe Adverse Events (TRSAE).
Patients included in arm 1 and in arm 0 will have the opportunity,according to their willingness, to receive either 1 (arm 1) or 1 or 2 (arm 0) MSC(AT) (2×10^6 cells/kg) injection(s) at the end of the study after unblinding and once evidence of MSC(AT) injection safety is provided.
Comparator treatment : Placebo
Number of subjects included : 18 patients
Number of sites : 2: Hôpital St Louis, Paris et CHU Toulouse
Duration of the trial
Inclusion period: 12 months
Participation period (treatment + follow-up): 12 months
Trial will have a Data Monitoring Committee:
Yes