- Autologous transplant procedure :
- Mobilization of Hematopoietic Stem Cells (HSC)
- Cytapheresis or Collection of Hematopoietic Stem Cells (HSC)
- Graft cryopreservation
- Pre-transplant conditioning
- Reinjection of Hematopoietic Stem Cells (HSC)
- Side effects and how to prevent them
- Hospitalization in a sterile room
- Psychological support
- Hospital discharge
- Follow-up schedule
- Vaccination instructions
Transplant procedure :
The transplant procedure for Hematopoietic Stem Cells (HSC) involves many steps :
Mobilization of Hematopoietic Stem Cells (HSC)
Mobilization and cytapheresis take place during a hospital stay of 10-15 days.
First, a central venous catheter will be placed: its function is to facilitate the administration of chemotherapy.
The mobilization phase begins with the administration of a one-hour infusion of chemotherapy, two days in a row. This chemotherapy usually induces a short period of aplasia.
A few days after the administration of chemotherapy, a hematopoietic growth factor (G-CSF) will be administered subcutaneously every day (between seven and ten days) until hematopoietic stem cells (HSC) are collected. :
This growth factor allows HSCs from the bone marrow to be released into the bloodstream.
Administration of hematopoietic growth factor (G-CSF) can lead to bone pain: you may be given medications to reduce this pain.
Cytapheresis or Collection of Hematopoietic Stem Cells (HSC)
The objective of this step is to collect hematopoietic stem cells (HSCs) from the bloodstream.
The collection is made by a simple technique called cytapheresis. Prior to this step, the nurses of the cytapheresis unit evaluate your vein integrity. If needed, a double-lane catheter will be placed near the groin crease just prior to collection and removed immediately afterwards.
The collection occurs in a cytapheresis unit. You are seated in a bed for duration of the procedure (between three and five hours) and a cell separator is located next to the head of the bed. The cell separator is a machine that separates the different cells types in your blood by a centrifugation technique. A sterile disposable kit is used at each cytapheresis session.
This machine will specifically collect the stem cells in your blood. Two veins are necessary for this technique: one allows the entry of blood into the separator, the other its return.
This collection can be repeated several days in a row (maximum of four days) until the number of collected stem cells collected is sufficient.
Graft cryopreservation
The hematopoietic stem cells (HSCs) that are collected from you are the graft. They are frozen and preserved in a cell therapy laboratory until the autologous transplant date
Pre-transplant conditioning
Pre-transplant conditioning takes place at least six weeks after hematopoietic stem cell (HSC) collection.
The pre-transplant conditioning regimen is an intensive treatment that is tailored to the condition being treated, your age, and your medical history. It consists of chemotherapy (4 days) with anti-lymphocyte serum (5 days). The goal of treatment is to eliminate “self-reactive” cells, the cells that cause your disease.
As a result of this chemotherapy, your body will have fewer white blood cells, red blood cells, and platelets: this is called aplasia. The duration of the period of aplasia varies between 10 and 15 days, depending on the person.
During this period, the risk of infection is increased because your body’s immune defenses are very weak. To limit this risk, you will be in a protected area (sterile room). Staff and visitors will wear a mask, a cap, and a hospital gown.
Reinjection of Hematopoietic Stem Cells (HSC)
After chemotherapy, your hematopoietic stem cells (the graft) are thawed in the cell therapy lab and reinjected into your blood stream. This process is called autologous transplant or autograft. The autologous HSC transplant is administered via your central venous catheter. The procedure lasts about 30 minutes to 1 hour, depending on the volume of the graft.
This procedure limits the period of aplasia by providing a source of new blood and immune cells that will replace the original immune cells eliminated by chemotherapy.
Side effects and their prevention
Conditioning chemotherapy may cause side effects, such as nausea, vomiting, disrupted gastrointestinal transit (diarrhea or constipation), mucositis (inflammation of the oral mucosa and throat), intense fatigue, hair loss, and risk of infertility. It also causes a period of aplasia. Blood transfusions are sometimes necessary to increase the red blood cell count.
The administration of the anti-lymphocyte serum may lead to flu-like symptomes (fever, pain, chills …).
Medications to fight against nausea, vomiting, and possible pain, you will be administered to prevent treatment side effects.
Before beginning treatment, your doctors will discuss fertility preservation techniques available to you and will suggest options.
Hospitalization in a sterile room
When hospitalized in a sterile room, the health care staff will strictly implement hygienic protocols. Instructions will be given to you and your family.
Daily living
It is recommended that you prepare certain personal items for your stay in a sterile room:
- Change of clothing for a minimum of seven days: seven outfits, underwear, and seven pajamas that can withstanding washing and ironing at 60 °. If you do not have someone who can handle your laundry, we will provide disposable clothing or hospital shirts during your stay
- jacket or fleece
- Indoor footwear: new or little used, and washed (if possible, two pairs: a pair of flip-flops and a pair of slippers)
- Toiletries: none (we will provide disposable towels and gloves, mouthwash and surgical toothbrush, moisturizer, and mild soap). Make-up and deodorant are not permitted
- Additional articles that are permitted: nail clippers, earplugs, night blinds, bedside lamp without fabric (plastic or metal)
- For men: electric razor
- For women: scarf, turban
- Avoid bringing jewelry, cash, checkbook …
- You will have at your disposal free television and WI-FI. You can bring your computer and tablet, as well as your cell phone.
You can also bring:
- DVD player, game consoles, radio /cd player, mp3 player …
- Book, magazine (preferably in its original plastic or from the middle of the pile and new)
- Personal photos, posters
- Personal documents in protective plastic sheet-cover, pens
- Sewing, knitting if new or very recent ball of yarn
On the other hand, newspapers or books made of recycled paper, plants, and cut flowers are not permitted.
Hygiene
You are asked to come on the day of admittance without any nail polish, or false nails.
During your hospital stay, we will ask you to attend to your daily hygiene with care, and to change clothes every day (pajamas included). A visit of a room can be organized before your stay, do not hesitate to contact us.
Visits
Visits are limited to two people in your room at the same time. Many visitors can still come the same day.
For the first visit, visitors will need to consult the health care team who will explain the hygiene protocol, including what protective clothing to wear. It is imperative that objects coming from “the outside” (computer, phone …) be entrusted to the nursing staff for cleaning before entering your room.
The presence of visitors is permitted during chemotherapy or during autografting.
Food
Before, during, and after your autograft special hygienic measures must be put in place in order to avoid any incidence of contamination from food. For these reasons, you will have routine follow-ups from the dieticians, who will adapt your diet and answer your questions.
In particular, prior to autologous hematopoietic transplant, your nutritional status is monitored to prevent undernutrition. Indeed, undernutrition prior to autografting increases the period of aplasia following the conditioning regimen.
Over the course of the transplant procedure, the side effects that you experience may result in insufficient calorie-nitrogen ratios. Your diet will be “protected” from risk of contamination from food, and adapted to your needs the side effects that you experience (potentially resorting to some degree of artificial diet).
When a freezer is available in the department, you can bring or have food brought to you under certain conditions: the quantity should be reasonable, in the form of food or industrial drinks (large area), in individual or reduced conditioning. In the case of frozen products, the transport time must be less than 20 minutes, in an insulated bag (its purchase is possible near the hospital). Home-made meat or baked products are prohibited.
At the time of discharge, your dietician, in consultation with the medical team, will give you advice on food hygiene.
Psychological support
This period of hospitalization can be difficult to accept and support. Talking about it can bring you comfort. A psychologist is available to you and your loved ones. If you want to meet with a psychologist, do not hesitate to make the request. If you are already followed by a psychologist in your referring center, your psychologist can maintain this relationship in the transplant unit.
Hospital discharge
Your time of discharge is determined by the medical team, based on your white blood cell count and overall condition. It is possible that prior to being able to return home, a continuation of hospitalization may be necessary in your referring center.
You will meet again with the dietician in the transplant unit a few days before your discharge. She will give you dietary advice for the return home and a dietary release booklet.
We advise you to avoid public places like shopping malls, public transportation, construction sites … etc. during the first three weeks following your hospital discharge.
In addition, it is recommended to wear a mask when traveling.
Details about the medical follow-up and the nursing care will be given to you when you leave, by the doctor and / or the referent nurse(s).
When you return home, you may experience some fatigue, including physical fatigue. This will decrease gradually over time. In consultation with the medical team, physical therapy may be prescribed. After your discharge, you will see a specialist from your referring center for follow-up.
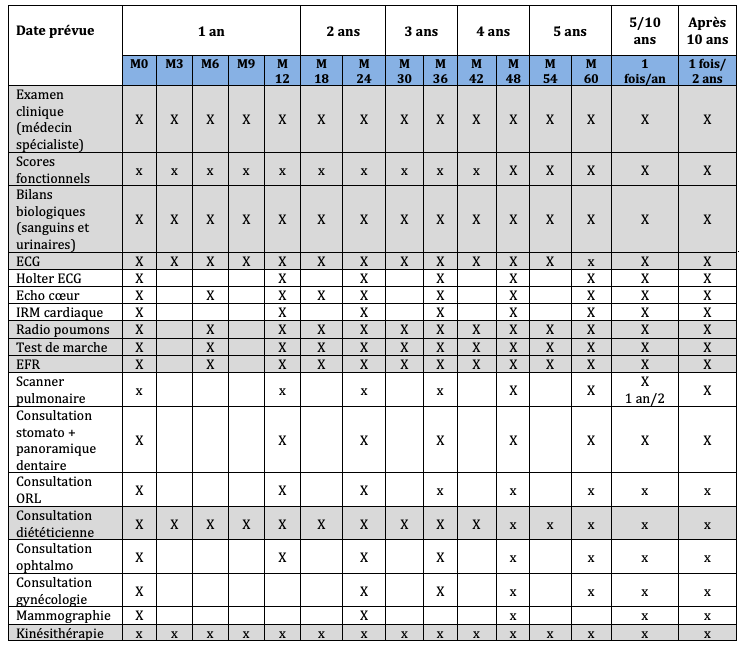
Follow-up schedule
Before your autologous hematopoietic stem cell transplant, a series of tests is done to evaluate your state of health. You will find the list in the table below.
The time of the pre-transplant assessment corresponds to column M0 (month zero). After transplantation, you will have regular follow-ups. In the first year, tests will be carried out every three months (M3, M6, M9, M12), during a a hospital stay. In some cases, these tests may be performed during in an outpatient setting.
After the first year, you will have tests every six months (M18, M24, M30, M36, M42, M48, M54, M60).
Tests in the gray rows are done at each follow-up visit.
Five years after the transplant, your tests will be conducted once per year. After ten years, they will be carried out every two years.
Vaccination instructions
After transplantation, some vaccinations will need to be done or redone. These will be spread out between the 6th and 24th month after transplant. There is no advantage in starting vaccinations before the third month post-transplant.
Vaccine recommendations: pneumococcal, diphtheria-tetanus-polio (DTP), haemophilus, whooping cough and hepatitis B, annual trivalent inactivated influenza vaccine, meningococcal C, hepatitis A (if traveling to countries where the disease is present), papillomavirus (6-12 months after transplant).
Vaccines that can be considered depending on the clinical context: chickenpox, measles-mumps-rubella (MMR), yellow fever.
The tuberculosis vaccine (BCG) and oral polio vaccine are contraindicated. The patient’s close entourage is advised to be up to date of its vaccines and to be vaccinated against the seasonal flu.
These vaccinations can be performed by your doctor or a nurse.